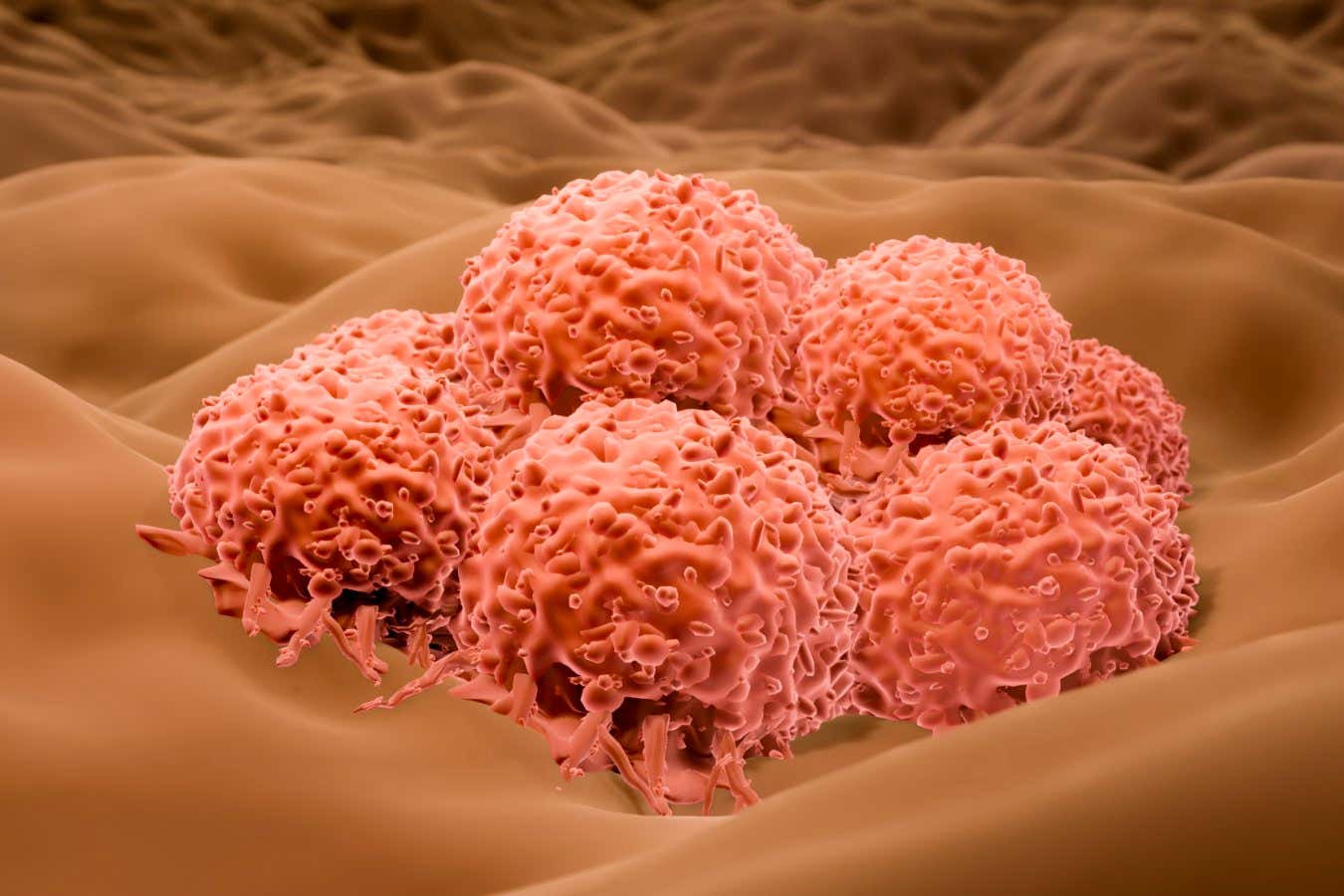
Melanoma is a type of skin cancer that can spread others in the body
Library’s photo science
Despite many decades of efforts and several human trials, only a virus is designed to kill cancers approved by regulators in the US and Europe. But one second could get the green light at the end of the month, after getting good results for treating melanoma, a particularly serious type of skin cancer.
A genetically modified herpes virus, called RP1, was injected into tumors of 140 people with advanced melanoma for which standard treatment had failed. Participants also took a drug called Nivolumab, which is designed to increase immunosfrom to tumors.
In 30 pr. Hundreds of the treated, shrinking tumors included those who were not injected. In half of these boxes, the tumors disappeared Altether.
“Half of the respondents had complete resorts, which means the complete disappearance of all tumors,” says Gino Kim at the University of Southern California. “We are very excited about these results.” The other options for treating people in this internship do not work and have more serious side effects, he says.
A study in later phase that will involve 400 people is now underway, but RP1 could be approved by Food and Drug Administration (FDA) in the US to treat advanced melanoma in combination with Nivolumab long before this trial is finished, told told told New scientist. “The FDA must give us a decision at the end of this month.”
It has been known for more than a century that viral infections can sometimes help treat cancers, but deliberately infecting people with “wild” viruses is very risky. In the 1990s, biologists genetically began to change viruses to try to make them better for the treatment of cancer and unable to damage healthy cells.
These viruses are designed to work in two ways. First, by directly infecting cancer cells and killing them by blasting them apart. Secondly, by triggering an immuno responsibility that is targeted at all cancer cells wherever they are in the body.
For example, a herpes simplex virusnown as T-WITH or Uigen penetration was modified to produce infed tumor cells to release an immune-stimulating factor called GM-CSF, among other changes. In 2015, T-WITH was approved in the US and Europe for the treatment of inoperable melanoma.
But T-MED is not widely used, you say, partly because it was only tested on and approved for injection into the skin tumors. Most people with advanced melanoma have deeper tumors, he says.
With RP1, a decision was made to also try to inject it into hair tumors. RP1 is a herpes simplex virus, as T-MED, but has been improved in number of ways. In particular, it causes the tumor cells to melt with nearby cells, help the virus spread through tumors and increase the immune response.
There have no direct comparable attempts with T-WITH and RP1, but RP1 is more likely to induce the shrinkage of all tumors, not only the injected, you say. “It indicates by a more powerful systemic effect.”
Therefore, in expectations, RP1 is much more widespread than T-MED if it is approved. It will also give a big boost to the whole idea of using cancerous viruses, he says. “I expect there to be much more interest.”
Topics: